Imagine a world where you struggle to find relief, where the simple act of passing stool becomes a source of discomfort and anxiety. This is the reality for millions of people living with constipation, a common yet often overlooked health concern. While constipation can be a frustrating and embarrassing condition, it’s important to remember that it’s treatable and a comprehensive nursing care plan can play a vital role in easing symptoms and restoring digestive health.

Image: www.scribd.com
Constipation is defined as infrequent bowel movements, hard stools, or difficulty passing stool. It can stem from various factors, including dietary deficiencies, lack of physical activity, medications, and underlying medical conditions. Understanding the underlying causes and implementing a personalized nursing care plan is crucial to address constipation effectively and promote overall well-being.
Understanding the Basics of Constipation
Constipation is not just about infrequent bowel movements. It involves a complex interplay of factors that affect how quickly waste moves through the digestive system. The key lies in the large intestine, also known as the colon, where water is absorbed from undigested food, forming stool.
In the case of constipation, the colon muscles contract sluggishly, and the stool becomes hard and dry, making it difficult to pass. Common symptoms include straining during bowel movements, feeling incomplete evacuation, abdominal discomfort, and bloating.
Causes of Constipation
The causes of constipation can range from dietary habits to underlying medical conditions. Here are some common culprits:
- Dietary Factors: A low-fiber diet lacking fruits, vegetables, and whole grains can contribute to constipation. Not staying adequately hydrated can also contribute to this issue.
- Lack of Physical Activity: Physical activity stimulates muscle contractions, including those in the digestive system. A sedentary lifestyle can slow down bowel movements.
- Medications: Certain medications, such as pain relievers, antacids, and antidepressants, can have constipation as a side effect.
- Medical Conditions: Constipation can be a symptom of underlying conditions like irritable bowel syndrome (IBS), hypothyroidism, and diabetes.
- Pregnancy: Hormonal changes and pressure on the intestines during pregnancy can lead to constipation.
- Stress and Anxiety: Stress and anxiety can disrupt normal digestive functioning, contributing to constipation.
Crafting a Nursing Care Plan: The Roadmap to Relief
A well-structured nursing care plan is essential for managing constipation effectively. It serves as a framework for addressing the underlying causes, monitoring progress, and implementing interventions to ease symptoms.
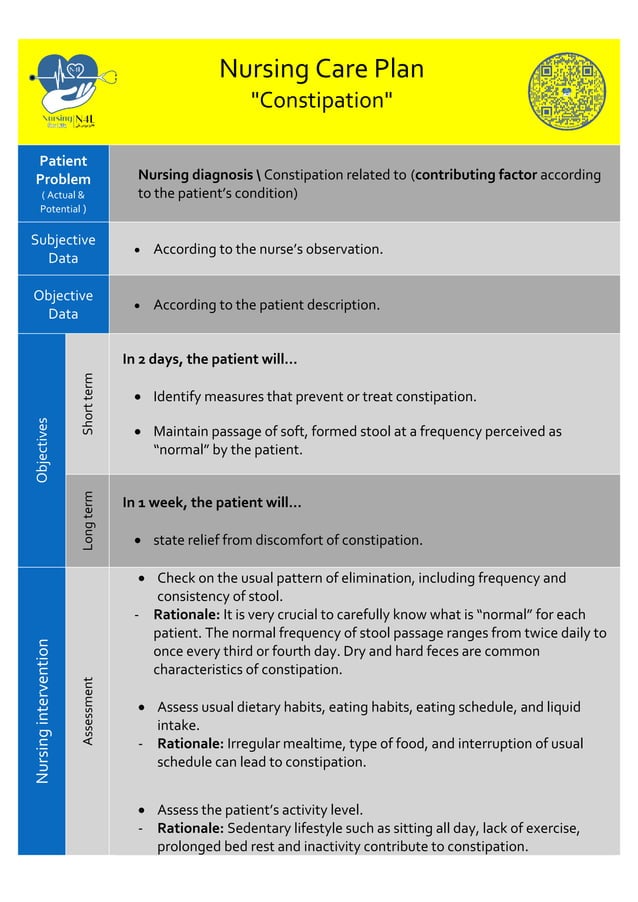
Image: www.slideshare.net
1. Assessment and Diagnosis: A Comprehensive Evaluation
The nursing care plan begins with a thorough assessment to identify the underlying cause and contributing factors of constipation. This involves:
- Patient History: Gather information about bowel habits, recent dietary changes, medications, and family history of constipation.
- Physical Examination: Assess the abdomen for distention, tenderness, or masses. The nurse may also assess the patient’s hydration status.
- Lab Tests: Some cases require laboratory tests, such as blood tests to check for thyroid function or electrolyte imbalances.
Based on the assessment, a diagnosis of constipation is established, and a personalized care plan is developed.
2. Medications: Supporting Bowel Function
Pharmacological interventions can be helpful in addressing constipation, particularly for cases resistant to lifestyle changes.
- Laxatives: Laxatives work by drawing water into the colon, softening the stool and promoting bowel movement. There are various types of laxatives available, including those that increase stool bulk (fiber supplements), those that soften the stool (stool softeners), and those that stimulate bowel contractions (stimulant laxatives).
- Stool Softeners: As their name suggests, stool softeners work by adding water to the stool, making it softer and easier to pass. These are often helpful for people with chronic constipation but are not particularly effective for acute constipation.
- Osmotic Laxatives: Osmotic laxatives work by drawing water into the intestines, thus softening the stool and stimulating bowel movements. They are effective for both acute and chronic constipation but can be associated with side effects like bloating or cramping.
- Stimulant Laxatives: Stimulant laxatives stimulate the muscles of the intestines, causing them to contract and move the stool along. These are effective for constipation but can lead to dependence with long-term use.
It’s crucial to understand that laxatives are not a long-term solution for constipation. They should be used under the guidance of a healthcare professional and only for a limited time.
3. Dietary Intervention: Fueling Digestive Health
Diet plays a crucial role in promoting regular bowel movements. The focus is on increasing fiber intake and ensuring adequate hydration.
- Increasing Fiber Intake: Fiber adds bulk to the stool, making it easier to pass. Good sources of fiber include fruits (berries, apples, pears), vegetables (broccoli, spinach, carrots), beans, lentils, whole grains, and nuts. It’s advisable to increase fiber intake gradually to avoid bloating and gas.
- Hydration: Water is essential for a healthy digestive system. Drinking plenty of water throughout the day helps soften the stool, making it easier to pass. Aim for at least eight glasses of water per day.
- Avoiding Constipation-Inducing Foods: It’s important to be mindful of certain foods that can worsen constipation. These include processed foods, red meat, refined grains, and sugary drinks.
4. Physical Activity: Getting Your Body Moving
Regular exercise is another crucial component of a nursing care plan for constipation. It stimulates muscle contractions, including those in the digestive system, promoting bowel movements.
- Types of Exercise: Any type of physical activity can benefit digestion. Walking, swimming, yoga, and cycling are excellent choices.
- Frequency and Duration: Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Lifestyle Modifications: Incorporate periods of movement into your daily routine. Get up and move around every hour or so, take the stairs instead of the elevator, or walk during your lunch break.
5. Bowel Training: Establishing a Regular Routine
Establishing a regular bowel training program can help retrain the digestive system to have more regular bowel movements. This involves:
- Setting a Regular Schedule: Choose a specific time each day, ideally after a meal, for bowel movements.
- Creating a Comfortable Environment: Find a quiet and private place where you can relax and focus on bowel movements.
- Positioning: Use a footstool or a slightly elevated toilet seat to help relax the muscles in the pelvic floor and make it easier to pass stool.
- Relaxation Techniques: Deep breathing exercises or progressive muscle relaxation can help relieve stress and promote bowel motility.
Bowel training can take time and requires consistency, but it can significantly improve bowel regularity over time.
6. Emotional and Psychological Support: Addressing the Emotional Impact
Constipation can have a significant impact on a person’s emotional well-being. It can lead to feelings of frustration, embarrassment, and anxiety. Therefore, it’s important to address these emotional aspects of the condition.
- Open Communication: Encourage open communication between the patient and the nurse about their concerns and feelings. This can help foster trust and build a stronger therapeutic relationship.
- Education and Reassurance: Provide accurate information about constipation and its management. This helps alleviate anxiety and demystify the condition.
- Support Groups: Connecting with others who understand the challenges of constipation can provide valuable emotional support.
Preventing Constipation: A Lifestyle Approach
The best approach to managing constipation is to adopt preventive measures to reduce the risk of developing it in the first place. This involves practicing a healthy lifestyle that includes:
- High-Fiber Diet: A high-fiber diet is cornerstone of preventing constipation. Focus on consuming plenty of fruits, vegetables, beans, lentils, and whole grains.
- Staying Hydrated: Drink plenty of water throughout the day, aiming for at least eight glasses. Other fluids, such as herbal teas and fruit juices, can also be beneficial.
- Regular Physical Activity: Incorporate regular physical activity into your routine. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Avoid Prolonged Sitting: Get up and move around every hour or so to prevent constipation associated with a sedentary lifestyle.
- Stress Management: Practice stress-reduction techniques, such as yoga, meditation, or deep breathing exercises. Stress can disrupt digestive function.
Nursing Care Plan Related To Constipation
Conclusion: Empowering Patients with Knowledge and Support
Constipation is a common and treatable condition that can be successfully managed with a comprehensive nursing care plan. By understanding the causes, implementing lifestyle modifications, and utilizing appropriate medications when necessary, patients can regain control over their digestive health. The nursing care plan provides a roadmap for addressing both the physical and emotional aspects of constipation, empowering patients to take an active role in their well-being. Remember, seeking professional guidance and maintaining open communication with a healthcare professional is vital for effective management and achieving long-term relief.






