Imagine a patient in the hospital setting, fists clenched, eyes blazing, and shouting threats. This, unfortunately, isn’t an uncommon scenario. Aggressive behavior in healthcare settings is a complex challenge that nurses face routinely. Understanding the root causes and implementing effective strategies is crucial to maintaining a safe environment for both patients and staff.
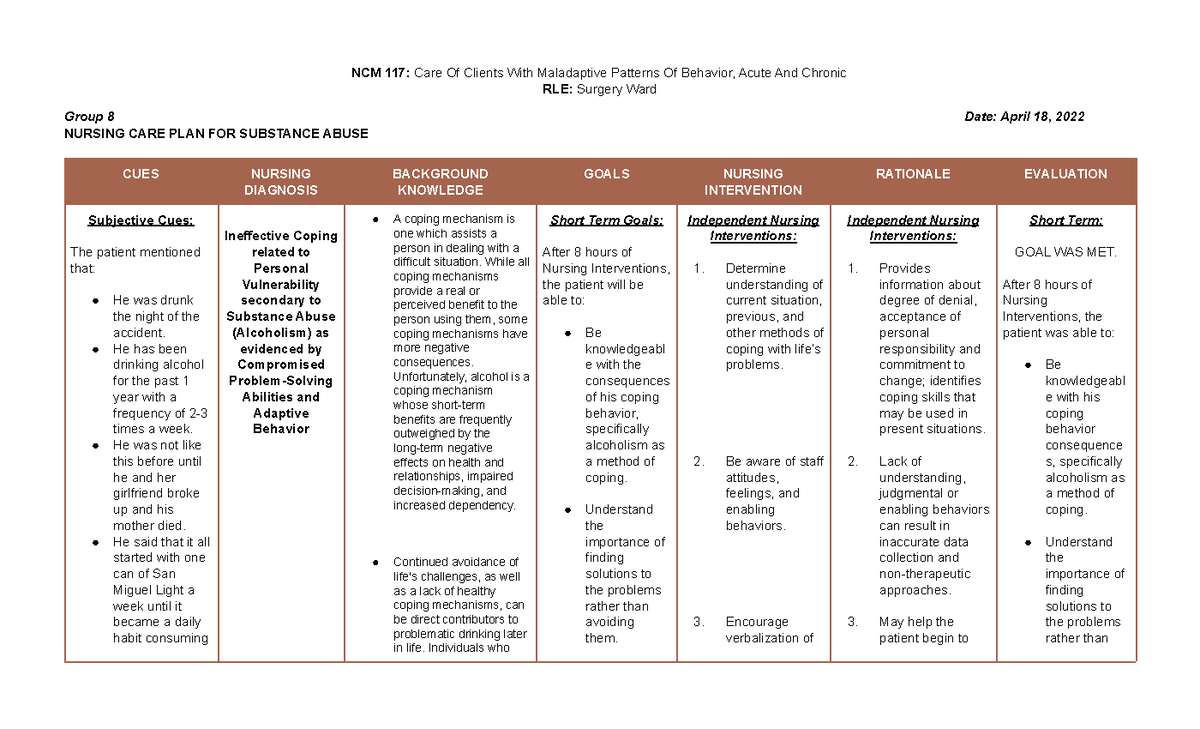
Image: www.vrogue.co
This article will delve into the intricacies of nursing care plans for aggressive behavior, providing a comprehensive roadmap for professionals to navigate this challenging terrain. We will explore the various causes, develop a framework for individualized care plans, and highlight essential techniques for de-escalation and preventing future episodes.
Understanding Aggressive Behavior in Healthcare Settings
Aggressive behavior in healthcare settings can manifest in diverse forms, ranging from verbal abuse and threats to physical assaults. It’s important to recognize that aggression is often a symptom of an underlying issue, and addressing the root cause is pivotal for effective management.
Common Causes of Aggressive Behavior
There are numerous factors that can contribute to aggressive behavior in patients. Understanding these underlying causes is essential for developing a tailored care plan:
- Medical Conditions: Neurological disorders such as dementia, brain injuries, and delirium can significantly impact cognitive function and emotional regulation, leading to outbursts.
- Mental Health Conditions: Patients with mental health conditions like schizophrenia, bipolar disorder, or depression may experience heightened emotions and aggression.
- Substance Abuse: Alcohol or drug withdrawal can trigger aggression due to physical discomfort and altered neurological functioning.
- Pain and Discomfort: Severe pain or discomfort can make individuals irritable and more prone to aggressive reactions.
- Environmental Factors: Overcrowding, noise, and lack of privacy can contribute to feelings of frustration and anxiety, potentially leading to aggression.
- Communication Barriers: Language differences, hearing impairments, or cognitive disabilities can lead to miscommunication and escalating tensions.
- Past Trauma: Individuals who have experienced past trauma, abuse, or neglect may be more likely to react aggressively to perceived threats.
- Medication Side Effects: Certain medications can cause side effects like irritability, agitation, or confusion, potentially triggering aggressive behavior.
Developing a Nursing Care Plan: A Step-by-Step Approach
A comprehensive nursing care plan for aggressive behavior is a vital tool for managing and reducing the risk of future episodes. Here’s a step-by-step approach to developing an effective plan:
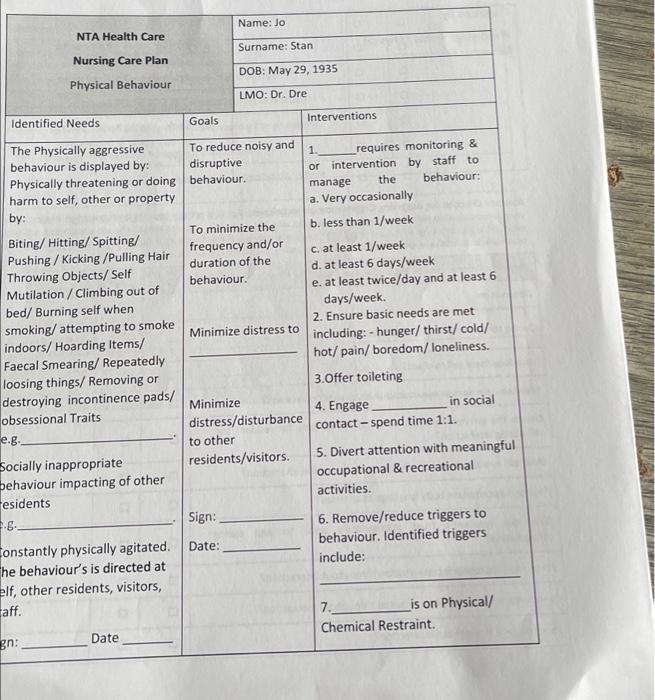
Image: www.chegg.com
Step 1: Assess the Situation
The first step involves a thorough assessment of the patient’s situation. This includes gathering essential information like:
- Medical History: Understanding the patient’s medical history, especially any preexisting conditions that may contribute to aggression.
- Mental Health History: Assessing any history of mental health disorders or current treatments.
- Substance Abuse History: Gathering information about past or current substance use, including alcohol or drug dependence.
- Current Medications: Identifying any medications the patient is taking, including any potential side effects.
- Environmental Factors: Evaluating the patient’s current environment, including noise levels, lighting, and crowding, to identify potential triggers.
- Patient’s Perception: Understanding the patient’s own perception of their aggression, if possible, can provide valuable insights.
Step 2: Identify Triggers and Prevention Strategies
Once you have a clear understanding of the contributing factors, you can begin identifying potential triggers. This involves analyzing the preceding events that may have led to the aggressive behavior. Common triggers include:
- Environmental Changes: Shifts in routines, unfamiliar environments, or sudden noise can trigger aggression.
- Physical Pain or Discomfort: Pain, discomfort, or unmet basic needs, such as hunger or thirst, can lead to outbursts.
- Social Isolation: Loneliness, lack of companionship, or perceived social rejection can contribute to aggression.
- Increased Demands: Feeling overwhelmed or unable to cope with expectations can trigger aggressive behavior.
- Frustration and Impatience: Delays in care, unmet needs, or feeling misunderstood can lead to frustration and aggression.
Based on identified triggers, develop preventative strategies that aim to minimize exposure to those triggers. This might include:
- Maintain Consistency: Stick to a consistent routine for the patient, such as regular mealtimes and medication administration schedules.
- Create a Calm Environment: Provide a quiet, well-lit environment with opportunities for privacy to reduce anxiety and frustration.
- Encourage Social Interaction: Encourage social interaction with family, friends, or staff to reduce feelings of isolation and loneliness.
- Use Clear and Simple Communication: Communicate clearly and concisely, using simple language and avoiding jargon to prevent misunderstandings.
- Provide Options and Choices: Give the patient choices whenever possible to empower them and reduce feelings of helplessness.
Step 3: De-Escalation Techniques
When aggressive behavior does occur, it is crucial to use de-escalation techniques to neutralize the situation safely and effectively. Here are some proven methods:
- Remain Calm and Professional: Maintaining a calm, professional demeanor sends a signal of reassurance to the agitated patient.
- Respect Personal Space: Avoid approaching the patient aggressively or invading their personal space. Allow them to calm down without feeling threatened.
- Use a Calm and Gentle Tone: Speak slowly, clearly, and respectfully, avoiding accusatory language or raising your voice.
- Active Listening: Attend to the patient’s verbal and nonverbal cues, acknowledge their concerns, and try to understand their perspective.
- Validate their Feelings: Validate the patient’s emotions, even if you disagree with their behavior. Saying, “I can see you’re feeling frustrated right now,” can help them feel heard and understood.
- Offer Choices: When possible, offer the patient options to regain some control over their situation. This could involve choosing a different seat, a specific drink, or a preferred method of communication.
- Distraction Techniques: Use distraction techniques to divert the patient’s attention from the trigger or source of frustration. This could involve redirecting their attention to a calming activity, like music, reading, or a conversation about a neutral topic.
Step 4: Documentation and Follow-Up
Thorough documentation is essential for tracking the patient’s progress and ensuring continuity of care. Record details of the aggressive behavior, including:
- Time and Date: Document the exact time and date of the incident.
- Circumstances: Describe the specific circumstances that led to the aggressive behavior.
- Patient’s Behavior: Detail the patient’s verbal and nonverbal behavior, including specific words used, tone of voice, and physical actions.
- De-escalation Measures: Record any de-escalation techniques used, their effectiveness, and the patient’s response.
- Outcome: Document the outcome of the situation, whether the aggression subsided, a specific intervention was required, or the patient was placed in restraints.
Regular follow-ups and evaluations of the care plan are crucial for ensuring its efficacy. The care plan should be periodically reviewed and adjusted based on the patient’s response, progress, and evolving needs.
Step 5: Seek Collaboration with Other Professionals
Sometimes, specialized expertise is required to address aggressive behavior. Collaborate with other professionals, such as:
- Psychiatrists and Psychologists: These professionals can diagnose and treat underlying mental health conditions that may be contributing to the aggression.
- Social Workers: Social workers can assess the patient’s social support network, environmental factors, and connect them with resources and services.
- Occupational Therapists: Occupational therapists can develop strategies for coping with frustration, managing stress, and enhancing daily living skills.
- Speech-Language Pathologists: These professionals can help the patient develop effective communication skills, improve their ability to express themselves, and minimize misunderstandings.
The Importance of Teamwork and Communication
The successful management of aggressive behavior relies heavily on effective teamwork and communication among healthcare professionals. It’s essential to:
- Share Information: Share relevant information about the patient’s history, triggers, and care plan with all team members.
- Coordinate Interventions: Work together to implement the care plan consistently, ensuring a consistent approach from all staff members.
- Open Communication: Foster open communication channels for sharing concerns, feedback, and updates on the patient’s progress.
- Regular Debriefing: Organize regular debriefing sessions to discuss challenging situations, analyze the effectiveness of care, and learn from past experiences.
Ethical Considerations in Nursing Care
When caring for patients exhibiting aggressive behavior, ethical considerations are paramount. Ensure that care is provided with:
- Respect and Dignity: Treat all patients with respect and dignity, regardless of their behavior.
- Least Restrictive Measures: Use the least restrictive methods for managing aggression, avoiding unnecessary restraint or seclusion.
- Patient Safety: Prioritize patient safety and protect them from harm, while also ensuring the safety of staff and other patients.
- Professional Conduct: Maintain a professional demeanor, avoiding personal judgment or retaliation, and focusing on de-escalating the situation.
Nursing Care Plan For Aggressive Behavior
Conclusion
Managing aggressive behavior in healthcare settings requires a comprehensive approach that considers the individual patient’s needs and triggers. By implementing a tailored nursing care plan, utilizing effective de-escalation techniques, and maintaining open communication among staff, professionals can create a safe and supportive environment for both patients and staff. Remember, every patient deserves compassionate care and the opportunity to receive the help they need to address underlying issues and reduce aggressive behavior.






