Have you ever watched a patient struggling to swallow, their lips parched and dry, their skin appearing taut and inelastic? These are some of the telltale signs of a fluid volume deficit, a common yet serious condition that can affect individuals of all ages and health statuses. As nurses, we play a pivotal role in accurately assessing, diagnosing, and managing fluid volume deficits to ensure the well-being of our patients.
Image: nandadiagnoses.com
This comprehensive guide will delve into the world of fluid volume deficit, covering its definition, causes, symptoms, nursing diagnoses, and interventions. Understanding this crucial nursing diagnosis empowers us to provide effective, compassionate care to patients experiencing fluid imbalance. Let’s embark on this journey together, gaining valuable insights that will enhance our critical thinking skills and clinical practice.
Defining Fluid Volume Deficit
A fluid volume deficit, also known as hypovolemia, refers to a state where the body’s total fluid volume is below normal. This can occur due to insufficient fluid intake, excessive fluid loss, or a combination of both factors. The severity of fluid volume deficit can range from mild dehydration to a life-threatening condition. It is crucial to promptly identify and address fluid deficits to prevent further complications.
Causes of Fluid Volume Deficit
The causes of fluid volume deficit are multifaceted and can stem from various physiological and environmental factors. Some common causes include:
1. Inadequate Fluid Intake
- Reduced thirst sensation: Conditions like dehydration, neurological disorders, and certain medications can impair thirst mechanisms, leading to decreased fluid intake.
- Conscious restriction of fluids: Some individuals may intentionally limit fluid intake due to various reasons, such as trying to lose weight or avoid unnecessary bathroom breaks.
- Inability to access fluids: Patients with limited mobility, impaired swallowing, or lack of access to clean water might struggle to consume adequate fluids.
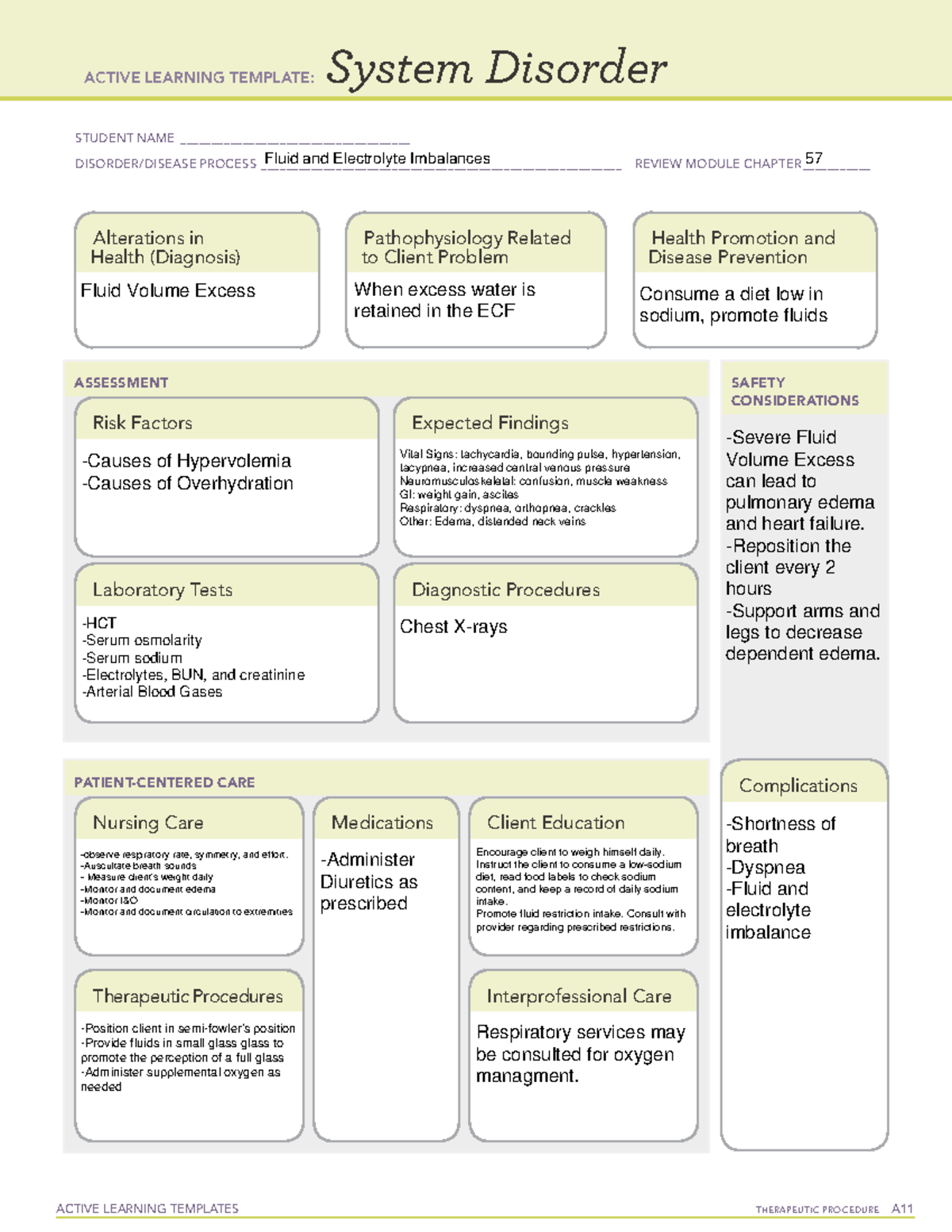
Image: mavink.com
2. Excessive Fluid Loss
- Gastrointestinal losses: Vomiting, diarrhea, and excessive sweating can lead to significant fluid loss.
- Urinary losses: Diuretic medications, kidney disease, and diabetes mellitus can increase urinary output, causing fluid deficit.
- Skin losses: Burns, open wounds, and fever contribute to fluid loss through increased perspiration.
Signs and Symptoms of Fluid Volume Deficit
Recognizing the signs and symptoms of fluid volume deficit is crucial for timely intervention. The body provides various signals, which may vary in intensity depending on the severity of the deficit. These include:
1. Cardiovascular Manifestations
- Decreased blood pressure: Hypovolemia reduces blood volume, leading to lower blood pressure.
- Weak, rapid pulse: The heart compensates for decreased blood volume by beating faster, resulting in a weak, rapid pulse.
- Orthostatic hypotension: A sudden drop in blood pressure upon standing, causing dizziness or lightheadedness.
2. Respiratory Manifestations
- Increased respiratory rate: The body tries to compensate for hypovolemia by increasing breathing rate to deliver more oxygen to tissues.
- Crackles or rales: Fluid buildup in the lungs, potentially leading to pulmonary edema, can be heard as crackles or rales during auscultation.
3. Neurological Manifestations
- Altered mental status: Confusion, lethargy, and delirium can occur due to decreased cerebral perfusion.
- Seizures: In severe cases, fluid deficit can lead to seizures due to electrolyte imbalances and decreased brain function.
4. Physical Signs
- Dry mucous membranes: The mouth, lips, and tongue become dry and sticky.
- Decreased skin turgor: The skin loses its elasticity and remains tented when pinched.
- Sunken eyes: Fluid loss can cause the eyes to appear sunken.
- Oliguria: Decreased urine output, usually below 30 ml/hour.
Nursing Diagnosis for Fluid Volume Deficit
Once we have established the presence of fluid volume deficit through careful assessment, we formulate a nursing diagnosis to guide our interventions. The most commonly used nursing diagnosis for fluid volume deficit is:
1. Deficient Fluid Volume
This diagnosis applies when the patient’s fluid intake is insufficient to meet their body’s needs. It is crucial to note that fluid volume deficit can occur even in the absence of visible signs of dehydration.
2. Risk for Deficient Fluid Volume
This diagnosis signifies a heightened risk of developing fluid volume deficit based on the patient’s specific factors, such as vomiting, diarrhea, or excessive sweating. Implementing preventive measures plays a critical role in preventing the development of this condition.
Nursing Interventions for Fluid Volume Deficit
Based on the nursing diagnosis, we implement specific interventions to correct fluid volume deficit and prevent its recurrence. These interventions can be categorized as follows:
1. Fluid Replacement
- Oral rehydration: Encourage patients to drink fluids regularly, taking into account individual preferences and fluid restrictions.
- Intravenous fluid therapy: Administer intravenous fluids, such as normal saline or lactated Ringer’s solution, as prescribed to rapidly restore fluid volume.
- Blood transfusions: In cases of severe anemia or blood loss, blood transfusions are administered to replenish lost red blood cells.
2. Monitoring Fluid Balance
- Intake and output: Accurately record all fluid intake (oral, intravenous, and other sources) and output (urine, vomitus, diarrhea, and drainage).
- Vital sign monitoring: Regularly assess blood pressure, pulse, and respiratory rate to detect changes in fluid status.
- Laboratory tests: Monitor electrolyte levels, blood urea nitrogen (BUN), and creatinine to assess fluid balance and kidney function.
3. Addressing Underlying Causes
- Treat underlying conditions: Identify and manage contributing factors, such as vomiting, diarrhea, or fever, to prevent further fluid loss.
- Medication adjustments: Consult with the healthcare provider to adjust medications that may contribute to fluid loss, such as diuretics.
- Nutritional support: Provide adequate nutrition to maintain energy levels and support healing.
4. Patient Education
- Teach patients about fluid volume deficit: Explain the importance of adequate fluid intake and the signs and symptoms of dehydration.
- Develop individualized fluid plans: Work with patients to create specific fluid intake goals tailored to their needs.
- Encourage regular follow-up care: Promote continued monitoring and seek medical attention if any concerning symptoms develop.
Nursing Diagnosis For Fluid Volume Deficit
Conclusion
Mastering the intricacies of fluid volume deficit is critical for nurses. By accurately assessing patients, formulating appropriate nursing diagnoses, and implementing effective interventions, we can prevent complications and promote optimal patient outcomes. This guide provides a framework for understanding this important nursing diagnosis, empowering you to provide the best possible care for your patients experiencing fluid imbalance. Remember, every patient is unique, and individualized care is key. Continue to expand your knowledge and skills by exploring additional resources and seeking ongoing education in this crucial area of nursing practice. Let’s strive to be vigilant advocates for our patients, ensuring their safety and well-being through informed, compassionate care.






