Have you ever wondered what makes the difference between a routine medical encounter and a truly impactful interaction with a healthcare professional? It’s not just about the clinical expertise; it’s about the relationship. In the world of nursing, building a strong therapeutic relationship is crucial for providing holistic care, promoting patient autonomy, and ultimately fostering healing. This article will delve into the four distinct phases of the therapeutic relationship, outlining the key elements of each and demonstrating how these phases work in tandem to create a supportive and therapeutic environment for patients.

Image: www.hosthealthcare.com
The therapeutic relationship in nursing is defined as a professional, collaborative, and trust-based connection between a nurse and their patient. It goes beyond simply delivering medical care; it encompasses active listening, empathy, respect, and shared decision-making. This relationship is more than just a means to an end; it’s a foundation for creating a safe and trusting space where patients feel empowered to participate in their care, navigate their emotions, and ultimately reach their health goals.
Phase 1: Orientation
Building the Foundation: Establishing Trust and Parameters
The orientation phase sets the stage for the therapeutic relationship. It’s where the nurse and patient first meet, embark on initial interactions, and lay the groundwork for future communication. During this phase, the nurse aims to:
- Establish rapport: Building an initial sense of trust and connection is vital. This involves introducing oneself clearly, using active listening skills, and demonstrating genuine interest in the patient’s well-being. A warm smile, a comfortable posture, and a gentle tone can make a substantial difference.
- Gather information: This phase involves asking relevant questions, reviewing medical history, and assessing current health concerns. Open-ended questions are key to encouraging the patient to share their story and perspective. For instance, instead of asking “How are you feeling?”, ask, “Can you tell me more about what brought you to the hospital today?”
- Set boundaries and expectations: It’s essential to establish clear boundaries right from the beginning. This includes outlining roles, confidentiality expectations, and the purpose of the therapeutic relationship, ensuring both parties understand the limitations and responsibilities involved.
- Identify the patient’s needs: This phase focuses on understanding the patient’s immediate needs, concerns, and goals. A nurse needs to actively listen to what the patient is saying, both verbally and nonverbally. Recognizing a patient’s unmet needs, whether social, emotional, or physical, is crucial to tailoring personalized care.
- Develop a plan of care: Based on the gathered information and established needs, the nurse collaborates with the patient to create an individualized plan of care. This involves setting realistic goals, explaining treatment options, and ensuring the patient understands their role in the process.
Phase 2: Working
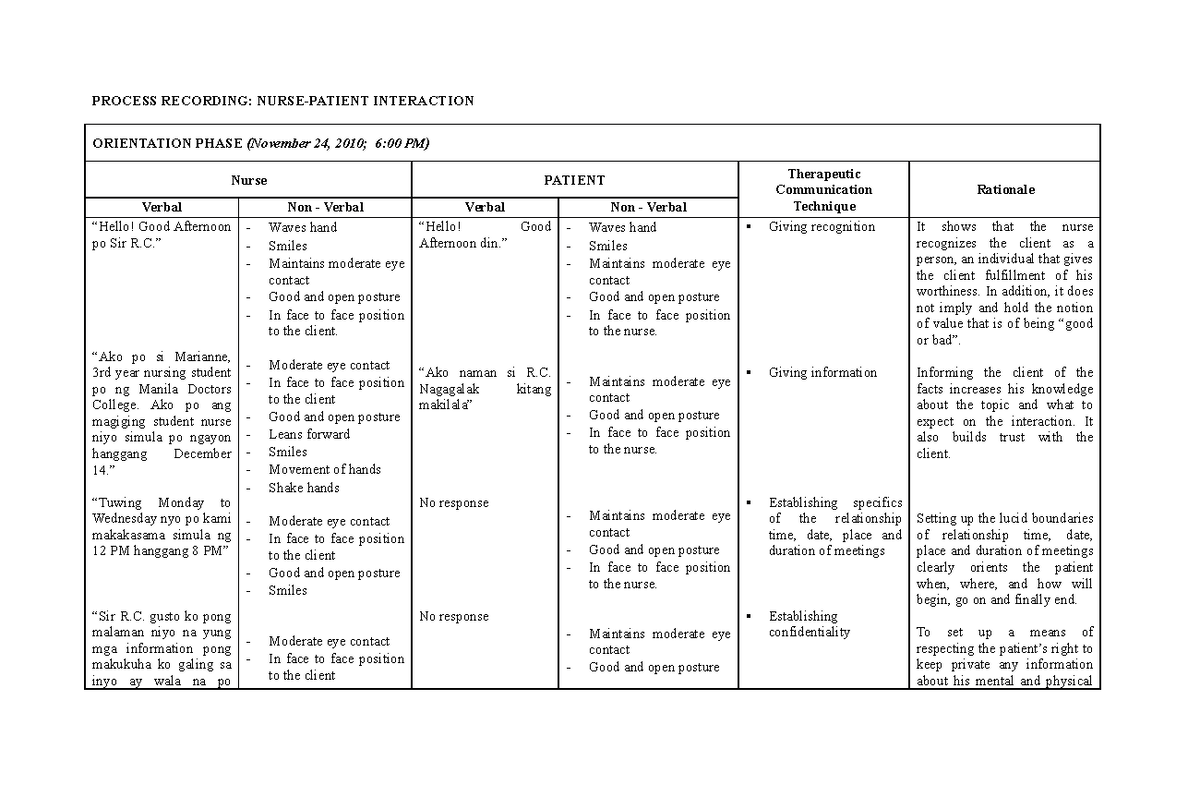
Image: www.studocu.com
Empowering Healing: Collaboration and Problem-Solving
The working phase is the heart of the therapeutic relationship, characterized by active collaboration and problem-solving. It’s during this time that the nurse and patient work together to achieve the predefined goals. Key elements of this phase include:
- Continued communication: Open and honest communication is essential throughout the working phase. It involves listening actively, asking clarifying questions, and providing feedback in a respectful and non-judgmental manner. This ensures that the patient feels heard and valued.
- Shared decision-making: Empowering patients to participate in their care is central to this phase. This involves explaining treatment options in clear language, encouraging questions, and respecting the patient’s choices, even when they may differ from the nurse’s recommendations.
- Problem-solving and coping mechanisms: This phase addresses challenges faced by the patient, including managing symptoms, coping with difficult emotions, and navigating various aspects of their illness. The nurse acts as a supportive guide, offering practical strategies, and teaching coping skills to help the patient manage their care and regain a sense of control.
- Building trust and confidence: As the working phase progresses, the nurse-patient bond strengthens. This involves demonstrating reliability, maintaining professionalism, and offering consistent support to build trust and foster a sense of security for the patient.
- Promoting independence: The ultimate goal is to empower the patient to become more independent in managing their health. This involves teaching self-care techniques, encouraging self-monitoring, and gradually transitioning the patient toward autonomy, while continuing to provide support and guidance.
Phase 3: Termination
Navigating the End: Closure and Transition
The termination phase marks the end of the formal therapeutic relationship. While it might seem like a simple transition, this phase requires careful consideration and sensitivity to handle the emotional dynamics involved. Key objectives of this phase include:
- Preparing for the end: As the patient’s health improves and they approach discharge, the nurse prepares them for the transition back home or to another level of care. This includes discussing plans, addressing concerns, and providing relevant resources to ensure a smooth and safe transition.
- Expressing gratitude: Acknowledging the journey shared during the therapeutic relationship is essential. Expressing gratitude for the patient’s trust, effort, and contribution to their recovery demonstrates respect and fosters a sense of closure.
- Reviewing progress: Reflecting on the achievements and changes accomplished during the therapeutic relationship helps to solidify the positive outcomes and reinforce the patient’s progress. It provides an opportunity to acknowledge their strengths and celebrate their successes.
- Addressing unresolved issues: This phase allows for addressing any remaining concerns or open questions. This ensures that the patient leaves with a sense of closure and satisfaction, knowing that all their needs have been adequately met.
- Supporting the transition: Providing guidance, resources, and support for the patient’s ongoing care is essential. This might involve connecting them with community services, facilitating referrals to specialists, or providing follow-up instructions. The goal is to ensure continued support as the patient transitions back to their life and manages their health on their own.
Phase 4: Evaluation
Reflecting on the Journey: Assessing Impact and Growth
While often not explicitly considered a phase, evaluation is an essential component of the therapeutic relationship, occurring throughout the process. It involves reflecting on the effectiveness of the interactions and identifying areas for improvement, ensuring ongoing quality of care and patient satisfaction.
The evaluation phase can be broken down into two key aspects:
- Patient Evaluation: How satisfied was the patient with the care received? Did they feel supported, heard, and empowered during the therapeutic process? Did the nurse effectively address their needs and facilitate their healing journey? This can be assessed through direct feedback, surveys, and observation of overall patient well-being.
- Nurse Self-Reflection: It is crucial for nurses to reflect on their interactions, assess their effectiveness in building rapport, fostering trust, and achieving therapeutic goals. This involves critically analyzing their communication style, problem-solving approaches, and their overall impact on the patient’s experience. This self-reflection leads to continuous professional development and growth.
The evaluation phase is crucial for ensuring the sustained quality of therapeutic relationships in nursing. By reflecting on both the patient’s experience and the nurse’s approach, we can identify areas for improvement, enhancing the effectiveness and positive impact of these therapeutic interactions.
Real-World Applications
Imagine a young woman named Sarah who has been diagnosed with a chronic illness. She enters the hospital, feeling overwhelmed and uncertain about her future. The nurse caring for her, Jenna, recognizes Sarah’s anxiety and actively listens to her fears and concerns. Jenna builds trust by sharing information about Sarah’s condition in plain language, making Sarah feel empowered to participate in decisions regarding her treatment. This marks the beginning of their therapeutic relationship, entering the orientation phase.
As Sarah’s treatment progresses, Jenna continues to be a source of support and guidance. She helps Sarah navigate the challenges of her illness, teaches her coping mechanisms for managing symptoms, and encourages her to set realistic goals for her recovery. Together they work through Sarah’s anxieties and empower her to take ownership of her health, demonstrating the working phase in action.
As Sarah’s condition improves, she begins to feel more confident and independent. Jenna prepares her for discharge, providing her with information about home care, connecting her with relevant community resources, and expressing her gratitude for the journey they have shared. This shift towards independence signifies the termination phase.
Through this ongoing process, Jenna reflects on her interactions with Sarah, assessing her effectiveness in building a therapeutic relationship and supporting Sarah’s healing journey. She considers how she might adjust her approach in the future to further empower patients and enhance the overall therapeutic experience. This demonstrates the essential role of continuous evaluation in improving the quality of therapeutic relationships.
4 Phases Of Therapeutic Relationship In Nursing
Conclusion
The four phases of the therapeutic relationship in nursing provide a framework for creating a supportive and healing environment for patients. By establishing trust, demonstrating empathy, and collaborating with patients in their care, nurses can create meaningful connections that foster healing and empower patients to take control of their health. The therapeutic relationship is not a linear progression but rather a dynamic process that requires ongoing learning, adaptation, and reflection. By embracing these phases, nurses can elevate the quality of care and significantly impact the lives of the patients they serve. To explore this topic further, consider researching various therapeutic communication techniques, patient-centered care models, and resources on building supportive relationships in healthcare.






