Imagine a world where every breath is a struggle, where simple tasks like walking to the mailbox leave you gasping for air. This is the reality for millions of people living with congestive heart failure (CHF). As a nurse, I’ve witnessed firsthand the challenges and triumphs of patients navigating this complex condition. The key to effective care lies in a well-structured nursing care plan, and this guide will walk you through the essentials, utilizing the visual power of Slideshare for a comprehensive understanding.
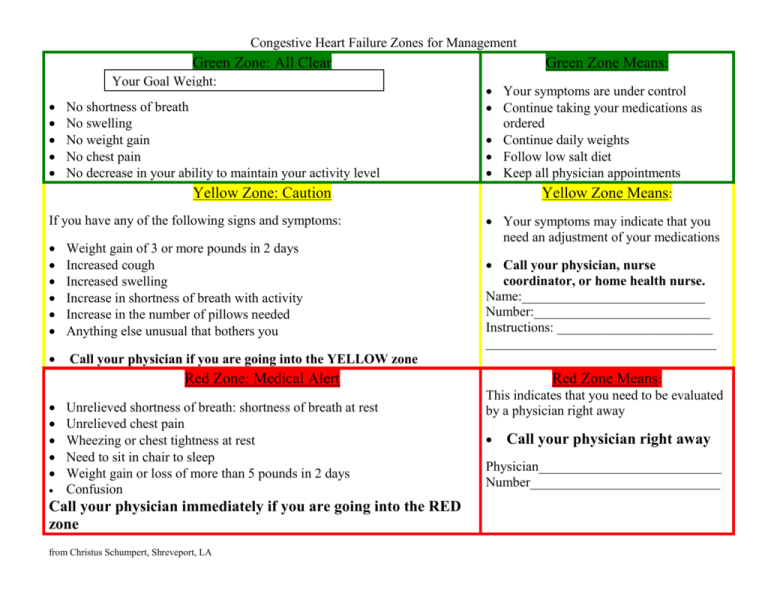
Image: studylib.net
CHF is a serious condition that affects the heart’s ability to pump blood effectively throughout the body. It can be a silent killer, with symptoms often showing up late. It’s crucial for nurses to have a robust understanding of the disease and a planned approach to provide the best possible care. The use of a robust nursing care plan, in conjunction with Slideshare, can be a powerful tool for organizing care and ensuring consistent, high-quality patient outcomes.
Understanding CHF: A Closer Look
Con congestive heart failure (CHF) occurs when the heart muscle weakens, making it difficult for the heart to pump blood efficiently throughout the body. As a result, blood can back up in the heart’s chambers, leading to fluid buildup in the lungs, legs, and other parts of the body. It’s important to understand that CHF is not a singular condition but rather a chronic disease with significant variations in severity and progression. This means that each patient’s care plan must be individualized to their needs and risk factors.
The causes of CHF range from heart attacks and coronary artery disease to high blood pressure, diabetes, and even certain infections. While there’s no cure for CHF, there are many effective treatments, including medications, lifestyle modifications, and sometimes even surgery, to manage the symptoms and slow its progression. This is where a well-defined nursing care plan becomes critical. It allows a nurse to understand the specific challenges a patient is facing and create a plan tailored to their individual needs.
The Nursing Care Plan: Your Roadmap to Effective Care
Assessment: The Foundation of Care
A comprehensive assessment is the cornerstone of any effective nursing care plan for CHF. This involves gathering a detailed understanding of the patient’s medical history, current symptoms, and overall health status. Key areas to focus on include:
- Vitals: Blood pressure, heart rate, respiratory rate, temperature. Elevated heart rate, irregular rhythms, and rapid breathing can be crucial indicators of CHF progression.
- Physical Assessment: Examine for signs of edema (fluid retention) in the legs, ankles, and feet. Auscultate (listen) for crackles in the lungs, indicative of fluid build-up.
- Cardiopulmonary Assessment: Assess for breathlessness at rest or with exertion, which can be a symptom of worsening CHF.
- Lifestyle Assessment: Gain insight into the patient’s diet, exercise habits, smoking status, and current medications and their impact on their CHF.
- Mental Health Assessment: Assess the patient’s ability to cope with theirCHF diagnosis. Ancillary support from social workers and mental health professionals may be required.

Image: www.researchgate.net
Planning: Defining Measurable Goals
After a thorough assessment, a comprehensive nursing care plan should be developed outlining specific, measurable, attainable, relevant, and time-bound (SMART) goals. Some crucial elements include:
- Medication Management: The care plan should outline the patient’s prescribed medications for CHF, including diuretics, ACE inhibitors, beta-blockers, and digoxin. Nurses should explain the purpose of each medication and educate patients on proper administration techniques, potential side effects, and the importance of taking medications consistently.
- Fluid and Sodium Restriction: Limiting fluid intake and sodium consumption is essential to manage fluid retention. The care plan should detail these restrictions and explain their rationale. Nurses can help patients with meal planning and provide dietary advice to aid in this aspect.
- Daily Weight Monitoring: Weight fluctuations can be an indicator of fluid accumulation. The care plan should include a daily weighing routine, and the nurse should educate the patient on how to accurately track their weight and report changes. This data is crucial in monitoring the effectiveness of the current care plan.
- Activity Management: Pace activities to avoid excessive exertion. The care plan should outline a gradual increase in activity levels tailored to the patient’s tolerance. Nurses can help patients with planning appropriate exercise routines and guide them in identifying warning signs such as shortness of breath or chest pain. Encourage participation in activities the patient enjoys and explain the importance of rest.
- Emotional Support: Provide empathy and understanding as patients cope with the challenges of CHF. Help them develop strategies to manage anxiety, depression, and feelings of helplessness. The care plan should outline resources available for emotional support and mental health counseling.
- Education and Self-Management Skills: Equip patients with the knowledge and skills to manage their CHF effectively. The care plan should include teaching about the disease, medication adherence, lifestyle modifications, and emergency signs and symptoms to watch for. Encourage patients to actively participate in their care and ask questions.
Implementation: Putting the Plan Into Action
The implementation phase of the nursing care plan is where the rubber meets the road. This is where the plan is executed, with nurses providing direct care, education, and support to the patient. Crucial components include:
- Medication Administration: Administer medications as prescribed, monitor for side effects, and educate patients about their medications, emphasizing the importance of adherence.
- Fluid and Sodium Restriction: Assist patients in following their fluid and sodium restrictions, providing guidance on meal planning and understanding the impact of different foods. Discuss alternative options for flavoring food, as salt can be a significant contributor to fluid retention.
- Monitoring: Closely monitor vital signs, including heart rate, blood pressure, respiratory rate, and temperature. Report any significant changes to the physician promptly.
- Oxygen Therapy: Administer oxygen therapy as needed, and monitor respiratory status closely.
- Patient Education: Provide ongoing education about CHF, medication management, lifestyle modifications, and self-care strategies.
- Emotional Support: Offer emotional support and encourage patients to express their feelings and concerns. Refer to mental health professionals, social workers, or support groups as needed.
Evaluation: Continuously Measuring Progress
Just like a well-tuned engine needs regular maintenance, the nursing care plan needs to be continuously evaluated to ensure its effectiveness. Does the patient understand their condition and the treatments? Is the plan achieving desired results? Are there any barriers to adherence? This process of regular evaluation allows for adjustments and refinements to the plan, ensuring it remains relevant and meeting the patient’s unique needs.
Here are some key areas to evaluate:
- Patient Outcomes: Are the patient’s symptoms improving? Are they achieving their goals? This can be determined by monitoring vitals, weight, exercise tolerance, and overall well-being.
- Medication Effectiveness: Are the medications effectively managing the CHF? Are there any side effects? Monitoring medication adherence and patient response to treatment is crucial.
- Patient Satisfaction: Is the patient satisfied with the care they are receiving? Are their needs being met? Open communication and patient feedback are vital.
Tips & Expert Advice
Here are some tips from my experience as a cardiac nurse to help you create a robust CHF nursing care plan:
- Collaborate: Working closely with the patient, their family, and other healthcare providers is crucial for developing an effective plan. This ensures that the patient’s goals and needs are at the forefront of the process.
- Use Visual Aids: Utilize Slideshare or other visual tools to explain complex medical information to patients. Pictures, diagrams, and videos can make complex concepts easier to understand and promote patient engagement in their care.
- Empower Patients: Encourage patients to involve themselves in their care. This includes knowing their medications, monitoring their weight, managing their diet, and understanding their symptoms. Empowerment fosters a sense of agency and encourages adherence to the care plan.
- Promote Positive Lifestyle Changes: Encourage patients to adopt healthy habits, including regular exercise, stress management, and a heart-healthy diet. This not only helps manage CHF symptoms but also improves overall quality of life.
- Address Emotional Concerns: CHF can be a challenging diagnosis to live with, both emotionally and physically. Provide emotional support, empathy, and guidance as patients navigate their condition and learn to manage their day-to-day life with CHF. Be available to listen, validate their feelings, and connect them with resources for mental health support.
Remember, the nursing care plan is a living document. It should be reviewed and updated as the patient’s condition changes. Open communication with the patient, their family, and other healthcare providers is key to ensuring the plan remains relevant and effective.
Frequently Asked Questions
**What are the common symptoms of congestive heart failure?**
Common symptoms of CHF include:
- Shortness of breath, especially with exertion or when lying down
- Fatigue and weakness
- Swelling in the legs, ankles, and feet
- Rapid or irregular heartbeat
- Weight gain (due to fluid retention)
- Coughing, especially at night
- Loss of appetite
**What are the different types of congestive heart failure?**
CHF is categorized into two main types:
- Systolic heart failure: The heart’s ability to pump blood out of the chamber is weakened.
- Diastolic heart failure: The heart cannot relax and fill properly with blood between beats.
**Can congestive heart failure be prevented?**
While not all cases of CHF are preventable, some lifestyle changes can lower risk:
- Maintain a healthy weight
- Manage your blood pressure
- Control your cholesterol levels
- Quit smoking
- Manage diabetes effectively
Congestive Heart Failure Nursing Care Plan Slideshare
Conclusion
Developing a comprehensive nursing care plan for patients with congestive heart failure is a highly skilled and essential aspect of providing quality healthcare. The key is to collaborate with patients, their families, and other healthcare professionals to create a tailored, individualized plan that addresses their unique needs. This plan should incorporate a thorough assessment, clearly defined goals, and a plan for implementing and evaluating the plan.
Use Slideshare to present visual aids, explaining complex medical information in a clear and engaging manner. By empowering patients to understand their condition and actively participate in their care, you can make a meaningful difference in their well-being, fostering their resilience and improving their quality of life.
Are you interested in learning more about CHF nursing care plans? Do you have any questions or experiences to share?






